Case Study on Cancer
Number of words: 3141
Cancer refers to the development of abnormal cells (due to mutated genes) that have the ability to divide uncontrollably, invade and effectively destroy the body’s healthy and normal tissue. The abnormal cells usually form a mass which are referred to as tumours which can then spread around the body in a process called metastasis. Prostate cancer (PC) are cancers of the prostate gland, which is part of the male reproductive system (1). The prostate is the site for the production of seminal fluid which has the role of transporting and nourishing the sperm (1). PC is thought to be one of the most common types of cancer in men and is the sixth highest cause of death in men (2). There are many different types of PC; Acinar adenocarcinoma is the most common type of PC which is responsible for most of the cases (3). This type is specifically restricted to the cells that line the prostate gland. It is important to note that acinar adenocarcinoma is also the most common form of cancer in the lung (3). Furthermore, other types include ductal adenocarcinoma, urothelial, squamous cell and small cell cancer (3).
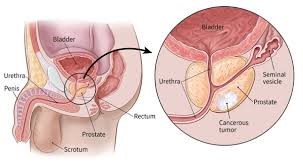
Figure 1 (4)- This diagram indicates where the prostate gland is situated, just below the bladder and anterior to the rectum. The urethra is the tube that goes through the prostate and carries urine (4).
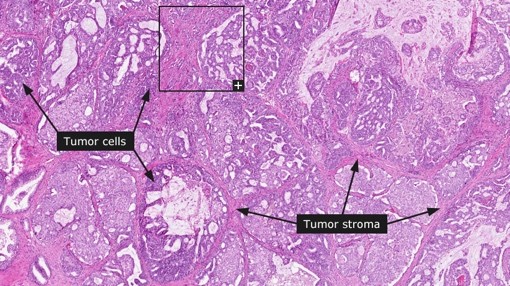
Figure 2 (5)- Histological diagram of PC and labelled tumours (5).
Unlike other cancers, PC does not always display signs or symptoms when it is in its early stages (1). An individual may have PC for several years and be unaware, this highlights the importance of regular screening for men. Those who are affected by this complication begin to experience symptoms when the tumour has had a direct effect on the prostate (causing it to grow) or has spread beyond the prostate. The following are examples of common symptoms, frequent urination especially during the night (which is what Joseph has been experiencing), blood in your urine or semen, pain or burning sensation when urinating, pain and or stiffness in your thighs and back and many more (6). It is vital to note that the mentioned symptoms are not of the caner itself but as a result of the growth of the cancer which blocks your prostate (6). As with many other cancers, PC also has many different stages. There is a specific staging system used in PC which is called TNM which is the abbreviation for tumour, node and metastasis (7). There are four stages in PC and stage four is the most vigorous and here it has spread to nearby organs, for example, the bladder or lymph nodes (7).
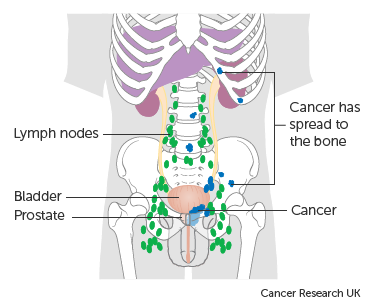
Figure 3 (7)- This illustration shows the that cancer has spread to nearby areas and outside of the pelvis (7).
In addition to the symptoms above, there are also symptoms which are specific to advanced PC, these include swelling and paralysis of lower body parts and many more in addition to these (6).
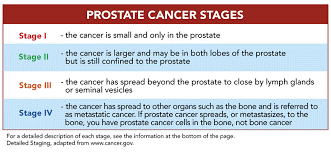
Figure 4 (8)- Table describing the different of PC (8).
In regard to the risk factors, there are a number of different variables which can increase a man’s risk in developing PC. Firstly, as the man’s age increases so does their chances of developing it (1). In fact, age is said to be the greatest risk factor. This is thought to be because as men age the cells that have mutated in the prostate begin to form quicker than the regular cells and thus assemble to form a tumour. In addition to this, race is also considered to be another factor that increases chances of developing the cancer. African American men tend to be more at risk of developing the cancer and when they are diagnosed, they often have a more advanced form of the cancer (1). Family history and obesity are also contributing factors (1).
Although the exact causes of PC are still somewhat unclear to scientists and clinicians, it is almost certain that genetics and environment both have a significant involvement (9). Men who have a brother or father who have PC are twice at risk relative to the those who do not (9). It has also been discovered that there is no single gene that is solely responsible for the condition (9). A Genetic Risk Score (GRS) is a new technology which uses high risk genetic markers to help identify the risk of those who have families with PC of also developing it (9). In addition to the genetic risks, the environment also plays an important role (9). There are links between the development of the disease and dietary habits of the western world. Those who have a high intake of saturated fats and milk produce have an increased risk, low vitamin D is also a contributor (9). Furthermore, consumption of certain vitamins may also increase the risk (9). Moreover, environmental exposure like some medication and medical procedures like the use of NSAIDs have shown to decrease the risk of PC. However other chemicals such as agent orange have been seen to increase chances of the recurrence specifically after surgery (9).
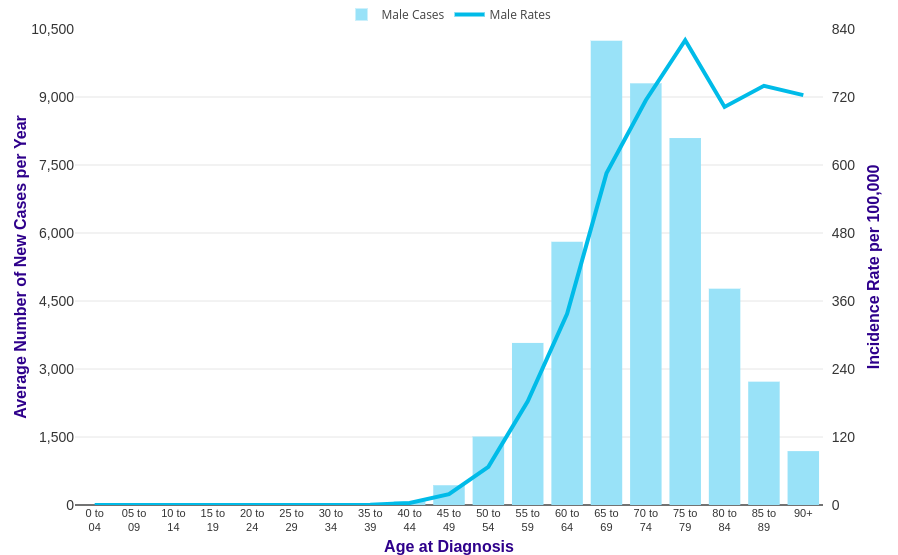
Figure 5 (10)- Graphical depiction of the cases of PC and age. As show the risk increases between 40 to 79 (10).
The diagnosis for PC includes two initial screening tests which include Digital rectal exam (DRE) and Prostate-specific antigen test (PSA (11)). In DRE, the physician examines the prostate for any irregularities in the shape or size. They do this by inserting a finger which is both gloved and lubricated. In addition to this, a PSA test may also be used (11). This includes taking a blood sample from the patient’s medial cubital vein (arm) and the PSA levels are then carefully monitored which is a substance made by the prostate (11). A small amount of the substance is normal, but a large amount has indications of infection or cancer (11). In relation to this case, Joseph’s PSA levels came back as 57ng/ml whereas the normal amount is less than 4ng/ml. If any abnormalities are detected following these tests, further examinations may be conducted. One method includes ultrasound (transrectal), here sound waves are used by the small probe to create a picture of the gland (11). Another method is collecting samples from the prostate of the tissue (prostate biopsy), this is done by inserting a thin needle into the prostate to collect tissue, it is then analysed in the lab to determine whether cancer cells are present (11). Lastly, an MRI fusion can also be used (this is still being worked on) (11). A different test may be used to determine how far the PC has advanced and its severity. If the results of the biopsy are positive, then it is essential to identify the stage of development (11).
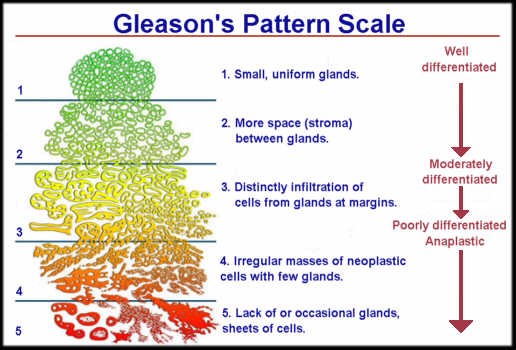
Figure 6 (12)- depiction of Gleason’s grading system and its relative differentiation rates (12). The most commonly used scale is called Gleason scoring system, in this two numbers (ranging from two to ten) nonaggressive and aggressive are combined (11). One benefit of this system is that it will allow for the appropriate treatment options which are tailored for that person. The scoring system works on the basis of assigning a primary grade to the largest area of the tumour and a secondary grade to the second largest area respectively (12). Thus, in Joseph’s case (3+4=7) means that grade 3 is most of the tumour and grade 4 is the next. As a higher number is suggestive that the cancer will grow faster, Joseph’s score indicates an intermediate risk for aggressive cancer (12). This is said to be better than a (4+3=7) score as it is less likely to spread (12).
Although PC is one of the most life-threatening diseases known to men, over the last twelve years early diagnoses and treatment has meant that the mortality rates have significantly dropped. Some examples of current medical treatments include surgery, radiation therapy, chemotherapy, hormonal therapy and many others. Although these methods may be effective, they don’t go without their negative side effects. Many of these treatments are not used as monotherapy but are a part of a collection of treatment plans. An example of this is the surgical removal of the prostate or prostatectomy. This treatment is more often recommended for high-risk locally advanced carcinoma. Prostatectomy has proved to be positive in preventing the risk of metastasis and thus progression and also reduces mortality (13). Those who have Gleason score ≤8 and PSA levels of <20ng/ml- this mode of treatment would not be suitable for Joseph (13). In addition to its benefits, there are also many adverse side effects of this treatment, firstly there are risks of lymph node metastasis and high rates of PSA recurrence (13). Other side effects include sterility which is caused by retrograde ejaculation and sometimes lymphedema (13).
Following a prostatectomy, radiotherapies often take place. The two types are external-beam radiotherapy (EBRT) and brachytherapy /internal radiation. Internal radiation is then further subcategorized into high dose and low dose (14). In high-dose rate brachytherapy, medical instruments such as catheters are inserted in the prostate (under anaesthesia) and a high level of radiation is administrated over a couple of minutes, usually in a few sessions (after the radiation is removed) (14). Conversely in low dose, specific seeds which hold radiation within them are placed in the gland (under anaesthesia) and the remain in the body and emit the radiation for a few months (14). In external therapy, for example, intensity-modulated radiation therapy is often co-administrated with hormone therapy (15).
In general, treatments like chemotherapy are not regarded as very effective against PC, having said that recent evidence proves that it is beneficial with hormone refractory PC, specifically it reduces pain and PSA levels (13). There are a few chemotherapeutic drugs used, examples of these include mitoxantrone, doxorubicin, vinblastine and many more (13). Mitoxantrone is an example of an anticancer antibiotic, this combined with prednisone (which is a prodrug) are what give the painkiller effects, despite this, they don’t improve the survival rate (13). The side effects of this treatment include fatigue, low blood cells and many more. The final mode of therapy is hormone therapy or androgen deprivation therapy. Androgens are a family of hormones that have a fundamental role in male traits and function by binding to androgen receptors and effectively energise the prostate tumour and help it grow (13). Hormone therapy essentially blocks the production of testosterone and prevents it reaching the prostate. Androgens bind a specific receptor called androgen receptors- this is a ligand dependent transcription factor, at normal levels androgens have minimal effect on the prostate, but the stimulation of the AR aids its growth. A very important part of this treatment is the blockage of different receptors and enzymes along this pathway (13). Unfortunately, this treatment does not go without its side effects, examples include loss of muscle mass, reduced libido, hot flashes and anaemia (13). Regarding Joseph’s case, the drugs given to him leuprorelin and flutamide are examples of non-steroidal anti-androgens oral drugs which both lower the testosterone level by inhibiting androgen production (it is a gonadotropin releasing hormone receptor agonist) (16).
An essential factor that determines your success rate of the treatment is dependent on the cancer stage that patient has. Physicians base the stage on three factors: the tumour size; metastasis and the chances of a relapse (17). In stage I, the cancer is relatively small and is contained within the prostate, it is also very slow growing and there may be no symptoms. The Gleason and PSA levels are quite low which is beneficial as the cancer is less likely to come back and it’s also less aggressive. Individual’s with stage I, may undergo active surveillance, where the doctor monitors the PSA levels, and if a rise is noticed he/she may decide for an alternative treatment. Radiation therapy may also be an option, this prevents the cells from growing and dividing (same as the radiation therapy mentioned above). And finally, surgical removal of the gland may also be considered. Moreover, what differentiates stage II from I is that the size of the cancer has increased, and the PSA and Gleason levels are also much higher, but the cancer is still contained within the prostate. In this instance, surgery and radiation are both needed, and a combination of radiation and hormone therapy may be use, this is important to stop the testosterone from aiding the cells to grow (similar to what Joseph had been given). Radical prostatectomy (RP) may also be performed.
Stage III and IV are more vigorous, and by stage IV it has reached the bladder, rectum and even lymph nodes. As these are often quite violent stages, the treatment must be more aggressive on the cancer. Often a combination therapy is given (of two or three), for example, RP, hormone therapy, radiation and even removal of lymph nodes situated in the pelvic region. Unfortunately, therapies often fail at stage IV, although treatments can reduce the pain. (17)
Figure 7 (18)- Stages of cancer, based on the Gleason score and description with possible treatment options (18).
Joseph’s relapse indicates that his initial treatment had not cured his disease and his raised PSA levels suggest that some of the cancer cells have survived. It is essential for Joseph to be retested following this event as it is likely for the cancer to have undergone metastasis and recurred in the neighbouring tissues (i.e. seminal vesicle). In Joseph’s case, it is likely that it has spread to his pelvis (as he is experiencing hip pains).
Figure 8 (19)- The line graph demonstrates the cure rate after radiation and the PSA levels. As shown, the probability of a relapse appears to be much less with the lowest probability being around 0.15 whereas the lowest rate of a man being cured and not experiencing a relapse i.e. PSA level below 2.5 is around 0.65. It is said the approximately 40% of men may experience a relapse (19).
Unfortunately, Joseph’s therapies have not been curative, and he has experienced resistance to the ADT (this mechanism is currently still not fully understood) (20). One reason may be the efflux mediated resistance, these pump the drug out of the cells and cause treatment failure (the application of nanoparticle-based platform is used to overcome this). Joseph’s AR have reactivated, and a second-generation AR drug is prescribed (20). As his cancer is likely to have spread to his bones (due to his hip pain), drugs such as LHRH agonists with anti-androgen drug (abiraterone) are effective (21). Alternatively, chemotherapy can be tried. Biphosphates and specifically Zoledronic acid, are drugs specific for PC spread to the bone, this is given intravenously and can relieve the pain (21).
In conclusion, it is vital for Joseph to start his new treatments immediately to prevent any further growth of the cancer. Although we cannot infer Joseph’s mortality rate from this data alone, a recent scientific trial states there is an 83.6% chance for a five-year survival rate following a recurrence (22). Despite this, further tests need to be conducted to prescribe treatment tailored to this patient to give maximum destruction of the cancer, pain relief and life expectancy.
Bibliography
Contributors M. PC – Symptoms and causes [Internet]. Mayo Clinic. 2019 [cited 29 November 2019]. Available from: https://www.mayoclinic.org/diseases-conditions/prostate-cancer/symptoms-causes/syc-20353087
Leslie S, Soon-Sutton T, Sajjad H, Siref L. PC [Internet]. Ncbi.nlm.nih.gov. 2019 [cited 29 November 2019]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470550/
Types and grades | PC | Cancer Research UK [Internet]. About-cancer.cancerresearchuk.org. 2019 [cited 29 November 2019]. Available from: https://about-cancer.cancerresearchuk.org/about-cancer/prostate-cancer/stages/types-grades
If You Have PC [Internet]. Cancer.org. 2019 [cited 29 November 2019]. Available from: https://www.cancer.org/cancer/prostate-cancer/if-you-have-prostate-cancer.html
Dictionary – Pathology: PC – The Human Protein Atlas [Internet]. Proteinatlas.org. 2019 [cited 29 November 2019]. Available from: https://www.proteinatlas.org/learn/dictionary/pathology/prostate+cancer+3
contributors W. PC Symptoms [Internet]. WebMD. 2019 [cited 30 November 2019]. Available from: https://www.webmd.com/prostate-cancer/guide/understanding-prostate-cancer-symptoms
contributors c. Number staging system | PC | Cancer Research UK [Internet]. Cancerresearchuk.org. 2016 [cited 30 November 2019]. Available from: https://www.cancerresearchuk.org/about-cancer/prostate-cancer/stages/number-staging-system
PC Staging and Grading [Internet]. ZERO – The End of PC. 2019 [cited 30 November 2019]. Available from: https://zerocancer.org/learn/newly-diagnosed/what-should-i-know/staging-and-grading/
Leslie S, Soon-Sutton T, Sajjad H, Siref L. PC [Internet]. Ncbi.nlm.nih.gov. 2019 [cited 30 November 2019]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470550/
contributors c. PC incidence statistics [Internet]. Cancer Research UK. 2019 [cited 30 November 2019]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/incidence
contributors M. PC – Diagnosis and treatment – Mayo Clinic [Internet]. Mayoclinic.org. 2019 [cited 30 November 2019]. Available from: https://www.mayoclinic.org/diseases-conditions/prostate-cancer/diagnosis-treatment/drc-20353093
Gleason Score [Internet]. Prostateconditions.org. 2019 [cited 30 November 2019]. Available from:
Fang-zhi C. PC: Current Treatment and Prevention Strategies [Internet]. pubmed. 2013 [cited 3 December 2019]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3785898/
Tontonoz M. What Every Man Should Know about Radiation Therapy for PC [Internet]. Memorial Sloan Kettering Cancer Center. 2016 [cited 3 December 2019]. Available from: https://www.mskcc.org/blog/what-every-man-should-know-about-radiation-therapy-prostate-cancer
Tontonoz M. Radiation Therapy for PC [Internet]. Memorial Sloan Kettering Cancer Center. 2016 [cited 3 December 2019]. Available from: https://www.mskcc.org/cancer-care/types/prostate/treatment/radiation-therapy
contributors c. Androgen deprivation therapy (ADT) for PC | EdCaN [Internet]. Edcan.org.au. 2019 [cited 3 December 2019]. Available from: http://edcan.org.au/edcan-learning-resources/case-based-learning-resources/prostate-cancer/active-treatment/androgen-deprivation
Contributors W. PC: Treatments by Stage [Internet]. WebMD. 2019 [cited 4 December 2019]. Available from: https://www.webmd.com/prostate-cancer/guide/treatments-by-stage#1
Kirandeep Panesar F. PC: An Overview of the Disease and Its Treatment [Internet]. Uspharmacist.com. 2010 [cited 4 December 2019]. Available from: https://www.uspharmacist.com/article/prostate-cancer-an-overview-of-the-disease-and-its-treatment
Postoperative Radiation for PC [Internet]. Aboutcancer.com. 2019 [cited 5 December 2019]. Available from: http://www.aboutcancer.com/prpostop1.htm
A B. Resistance to Hormonal Therapy in PC. – PubMed – NCBI [Internet]. Ncbi.nlm.nih.gov. 2019 [cited 5 December 2019]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28353036
Contributors A. Treating PC That Doesn’t Go Away or Comes Back After Treatment [Internet]. Cancer.org. 2019 [cited 5 December 2019]. Available from: https://www.cancer.org/cancer/prostate-cancer/treating/recurrence.html
Dell’Oglio P e. Predicting survival of men with recurrent PC after radical prostatectomy. – PubMed – NCBI [Internet]. Ncbi.nlm.nih.gov. 2019 [cited 5 December 2019]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26707594