Essay on Mental Health and Substance Use Disorder
Number of words: 2233
INTRODUCTION
Mental health and substance use disorders are significant public health concerns that often co-occur with violence. In order to understand, address and improve concerns related to mental health and substance use disorders, it is critical to analyze perspectives of people who are affected and have sought help for substance use disorders. These people serve as service users of substance disorders. Any attempt to judge the experiences of health services without considering the experiences of people involved in their use would be incomplete. Through finding out what service users experience, drawing conclusions, and delivering a solution is made more accessible. This paper focuses on an individual’s life experiences (named Tyson) with severe substance use disorders and requires specialty treatment.
According to Canadian Center on Substance Use and Addiction (2014), a substance use disorder is characterized by clinically significant impairments in social functioning, health, and voluntary control over substance use. Substance use disorders range from mild to severe with respect to the severity and duration of their existence. Therefore, a mental illness is simply a disease/illness that changes a person’s thinking, behavior, and feelings and perhaps leads to distress and difficulty in functioning Canadian Center on Substance Use and Addiction (2014). Notably, a person with a mental illness does not necessarily look sick, especially when their condition is mild. This paper describes the critical components of a substance use disorder service user by determining their symptoms, challenges they incur, and the support the service users receive from SSW or MHAW considerations.
RECOGNIZING
We can all be sad or blue at some point in our lives; we have seen madmen and people of the kind in real life and movies and animations. This case presents an actual person with explicit symptoms of mental illness and substance use disorder such as confusion, agitation, and withdrawal. Other illnesses experienced by Tyson include schizophrenia, autism, depression, attention deficit hyperactivity disorder (ADHD), among other obsessive-compulsive disorders. However, it is essential to note that not all brain diseases are categorized as mental illness or substance use disorder. Neurological diseases such as epilepsy and Parkinson’s are brain disorders but do not qualify as mental illnesses Canadian Center on Substance Use and Addiction (2014).
Signs, symptoms, and behavior of Mental Health Illness
Each mental illness has its characteristics; however, there are some general warnings/conditions/behaviors that can alert you that a person requires a professional health check-up. According to the service user of a substance use disorder, the condition of mental wellbeing often changes and co-occur with issues related to substance use; these issues commonly intersect with trauma and violent experiences. That is, although the vast majority who have psychological well-being/substance use issues are not vicious, proof shows higher paces off at various times misuse and injury in their lives just as a current or on-going accomplice and non-accomplice animosity both as casualties and culprits, contrasted and people who do not have emotional well-being, or substance use issues.
Proof likewise shows that the two casualties and culprits of spousal maltreatment have more unfortunate emotional wellness than do the individuals who don’t encounter accomplice savagery. The co-event of psychological wellness, substance use, and savagery issues makes administration needs mind-boggling and requires exhaustive and facilitated care. To adjust administrations to the necessities of people who face issues, particularly the individuals who have simultaneous issues, analysts and experts require a superior comprehension of the encounters and points of view of individuals who have looked for help for just as the viewpoints of their relatives. Some mental health illness signs include;
- Marked personality change
- Excessive anger, violent or hostility behavior
- Prolonged depression and apathy
- Strange or grandiose ideas
- Excessive anxieties
- Mood swings which are extremely high or low
- Drug and alcohol abuse
- Inability to cope with problems and other daily activities
- The service user often talks about suicide or harming oneself
- Changes in sleeping and eating patterns
The above signs have great and psychological effects on Tyson, the service user, in a number of ways. For instance, the user’s daily chores are associated with very strange, impossible, and grandiose ideas such as exaggerating a lot about himself, his achievements, and his capabilities. Also, on many occasions, Tyson is spotted dismissing other people’s achievements and talents. Moreover, constant boasting and talking about himself brings irrelevancy to the service user.
If not enough, the service user experiences prolonged apathy and depression. This is categorized by Tyson’s disinterest in life activities and interactions with others. It has affected his ability to make friends, keep his duties and job well done, and no enjoyment of life at all cost. Tyson is not motivated to carry out his wellbeing, such as keeping neat and clean. Nevertheless, depression has reduced the quality of the user’s life with increased work and family problems. Today, Tyson is a low esteemed individual who underrates himself and finds isolation. Persistent depression and marked personality change have led to the following on service users;
- Loss of interest in day-by-day exercises
- Pity, void, or feeling down
- Misery
- Sluggishness and absence of energy
- Low confidence, self-analysis, or feeling unfit
- Inconvenience thinking and instigating choices
- Crabbiness or unnecessary displeasure
- Diminished action, viability, and efficiency
- Evasion of social exercises
- Sensations of blame and stress over the past
- Helpless hunger or gorging
- Rest issues
Biggest challenges
- Social interaction
According to Tyson, my greatest challenge is acting or responding in a manner considered socially satisfactory, for example, not getting irritated, inpatient, or furious. Defeating trepidation and uneasiness when managing new individuals is additionally a test, and not closing down and going into defensive battle mode. Similarly, I battle to interface with individuals with whom I share little for all intents and purpose, and sometimes, I neglect to see the worth in that.
- Making yourself a priority.
At the point when things are going admirably, life disrupts everything – work, family, companions. I love every one of them, so saying no is hard. At the point when I become self-satisfied and stop my ordinary practices, it’s right around an assurance that my temperament will change and go downhill. Getting sufficient rest and taking a walk are necessities, regardless of how bustling I am and how acceptable I’m feeling.
- Identifying moods and feelings
A major test isn’t knowing whether I’m feeling is identified with my disease, side effects, or simply a piece of life. Due to an arrangement change at work, I have been on decreased hours. Subsequently, I thought it was not easy to persuade myself to work at home and be useful. Is this suggestive of my disease? Or then again, is it related to sensations of misfortune and uncertainty over my future, and consequently typical? I re-think myself a great deal as a result of my sickness.
- Maintaining good routines
- Reaching out
- Planning and navigating the world
- Living up to expectations
RESPONDING
Social Service Worker’s (SSW) support
According to The role of social work in mental health (2019), most mental health settings remember administrations for three-wide degrees of medical care application: avoidance, therapy, and recovery. It is perceived that singular social specialists might rehearse only inside one defining or cross the limits of each of the three in light of assorted customer, family, and local area needs.
- Prevention
Plans to diminish the frequency of infection or brokenness in a populace through changing distressing conditions and reinforcing the capacity of the person to adapt. Counteraction includes the advancement and upkeep of good wellbeing through training, consideration regarding sufficient principles for fundamental requirements, and explicit security against known dangers.
- Treatment:
Plans to diminish the pervasiveness (number of existing instances) of a problem or brokenness and incorporates early conclusion, mediation, and treatment. In psychological well-being settings, treatment exercises are centered around people encountering intense mental manifestations, passionate injury, relationship issues, stress, pain, or emergency and incorporate evaluation, hazard the executives, singular, couple, family and gathering directing, intercession or treatment and backing. Social work utilizes relationships as the premise.
- Rehabilitation:
Targets diminish the delayed consequences of confusion or brokenness and include the arrangement of administrations for pre-preparing and recovery to guarantee the person’s most extreme utilization of residual limits.
Specific to their employment setting, social workers in mental health deliver the following professional services:
- Direct services
- Case management
- Community development
- Supervision and consultation
- Program management and administration
- Teaching
- Research and evaluation
- Social action
Evidence-based interventions
The evidence-based treatment turned into a well-known expression during the 1990s as mental health came to esteem the utilization of the logical strategy. While psychological well-being customarily had depended on emotional reports of clinical adequacy, advisors and other psychological well-being experts started calling for thorough examinations to be done to decide the viability of medicines and how to execute the best. The practices that went through thorough testing and were demonstrated with clinical and logical proof became known as evidence-based. The high bar that was set with the emphasis on the logical technique has brought about a sensational expansion in the viability of treatment. We’re done depending on the mystery. Hitched with patient inclinations and an advisor’s encounter, evidence-based practices are important apparatuses that can be utilized with certainty. Examples of evidence-based interventions include;
- Cognitive Behavioral Therapy
Works by assisting individuals with recognizing and changing perplexing and dreary examples of reasoning imbued over numerous years, influencing feelings and driving conduct. CBT is an intercession strategy that changes the manner in which customers ponder themselves and their environmental elements Health care systems and substance use disorders – Facing addiction in America (2016).
- Dialectical behavior therapy
Dialectical behavior therapy is a cognitive behavioral therapy that gives a more prominent spotlight on friendly and enthusiastic components. It was created to approach to assist individuals with outrageous or shaky feelings and hurtful reckless practices.
- Exposure therapy
- Functional Family Therapy
- Assertive Community Treatment
- Motivational Interviewing
RESOURCES
RECOVERY ORIENTATION
The recovery dimension-oriented practice includes the following;
- Creating a culture and language of hope
Recovery is workable for everybody. Expectation animates recovery, and gaining the capacities to support trust is the beginning stage for building an emotional wellness framework outfitted to cultivating recuperation (Gutierrez, 2020, P 220-223). In this sense, recovery is essentially about trust. This part contains a solitary, all-encompassing Rule that depicts how to convey positive assumptions and advance expectation and confidence to make an assistance culture and language that prompts an individual to feel esteemed, significant, invited, and safe.
- Recovery is personal
The key to recovery includes identifying each person’s uniqueness and their ability to determine their problem.
- Recovery occurs in the context of one’s life.
- Responding to the diverse needs of everyone living in Canada
- Recovery is about transforming services and systems.
Stigma and discrimination can make someone’s mental health worse. The best way to challenge this stigmatization is by doing the following.
- Talking about it openly and often.
- Educating oneself and others in the society (Gutierrez, 2020, P 227).
- Showing compassion to individuals with this problem.
- Encourage equality and equity.
Conclusion
Conclusively, mental illness is a manageable disease/disorder. Many individuals fall into the jaws of this menace due to lack of knowledge and space for expression. Creating a culture and language of hope is identified as various recovery procedures that assist in beating this disease. Moreover, adequate care and monitoring is advised to such individuals.
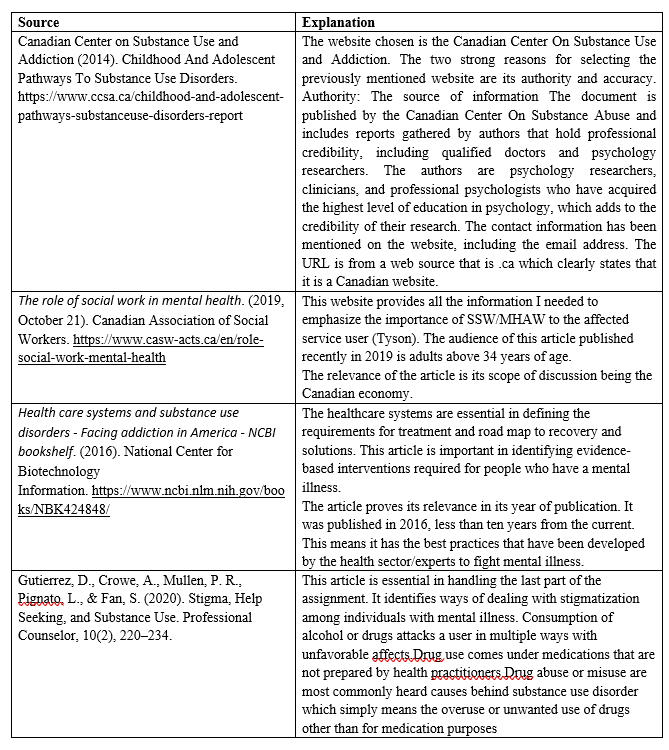
References
Canadian Center on Substance Use and Addiction (2014). Childhood And Adolescent Pathways To Substance Use Disorders. https://www.ccsa.ca/childhood-and-adolescent-pathways-substanceuse-disorders-report.
Gutierrez, D., Crowe, A., Mullen, P. R., Pignato, L., & Fan, S. (2020). Stigma, Help Seeking, and Substance Use. Professional Counselor, 10(2), 220–234.
Health care systems and substance use disorders – Facing addiction in America – NCBI bookshelf. (2016). National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK424848/
The role of social work in mental health. (2019, October 21). Canadian Association of Social Workers. https://www.casw-acts.ca/en/role-social-work-mental-health.